JHS Journal Club
Created in 2018, the JHS Journal Club is an online journal club that allows you to interact with other Journal of Hand Surgery readers from around the world and discuss interesting articles in JHS.
Formerly a Twitter/X-based discussion, the #JHSJC will now take place on Discord. Discord is a user-friendly virtual community where journal discussions can happen in real time and previous discussion transcripts can be archived.
How to Participate:
Step 1. Create your free account here by accepting this invitation. After you create an account, you’ll be sent directly to the discussion. If you already have an account, select the “Already have an account?” option and log in with your existing credentials on this invite. You can access this invitation on both your desktop computer or with the mobile application (search for “Discord,” available on both iOS and Android devices).
Step 2. Join the discussion! Post your thoughts in the text box at the bottom and you’ll see the conversation unfold in a standard “chat room” form. Note: If you are using the mobile application, log in and swipe right to see the discussion.
Questions? Contact us at jhs@assh.org.
The next #JHSJC is
Tuesday, June 11
8:00 PM Central / 9:00 PM Eastern

Article #1
Advancements in de Quervain Tenosynovitis Management: A Comprehensive Network Meta-Analysis
By Han Hong Chong, MBChB, MSc, Akhilesh Pradhan, BSc (Hons), MBBS, Mohit Dhingra, BMedSci, MBChB, William Liong, MS, Melinda Y.T. Hau, MBChB, iBSc (Hons), and Rohi Shah, BMBS, MSc SEM
DOI: https://doi.org/10.1016/j.jhsa.2024.03.003
Summary
The authors used an advanced approach to literature synthesis to allow comparison of results for the non-operative treatment of DeQuervain tenosynovitis, across a variety of non-operative treatments. The fundamental difference between this strategy and a meta-analysis is that the latter usually only compares two interventions, while the network meta-analysis allows comparison between many different interventions. They identified 14 randomized trials encompassing 823 patients. The outcomes were a visual analog pain scale and the DASH. In the short-term extracorporeal shock wave treatment showed improvement in pain scores compared to placebo. Corticosteroid injection alone, platelet-rich plasma injections alone, acupuncture, and splinting alone did not significantly differ from placebo in visual analog scale pain score. In the long-term (one year), CSI alone and platelet-rich plasma injections demonstrated sustained pain relief. Combining CSI with orthosis also appeared promising when compared with CSI alone.
Points for discussion
- This should rep[resent the best evidence available on this topic (most of the studies were considered low risk of bias). Do the findings ring true? If not, why not?
- In the short-term PRP (and many other treatments) didn’t differ from placebo, but in the longer-term, one years, corticosteroid alone and PRP were the only treatments with sustained relief. Does that reflect something about the proposed mechanism of action of PRP?
- Even though extra-corporeal shock wave treatment had the highest effect re: pain relief, in the short-term, corticosteroid and splinting ranked highly and in the longer term had the best results. What does that suggest as far as how the condition should be managed – especially since there is little evidence of a role for surgery and the condition is well-known to be self-limited in most cases.
Article #2
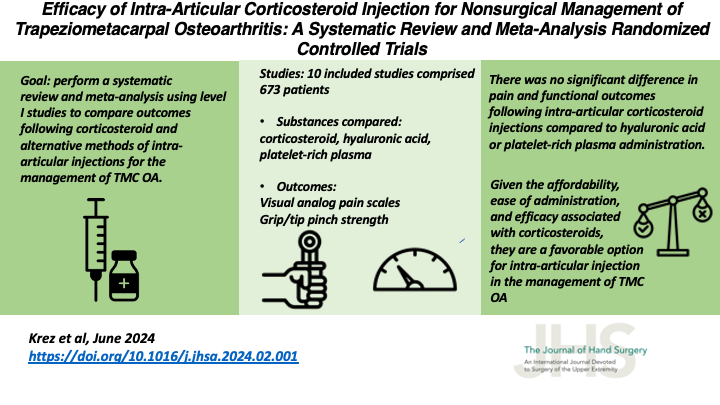
Efficacy of Intra-Articular Corticosteroid Injection for Nonsurgical Management of Trapeziometacarpal Osteoarthritis: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
By Alexandra N. Krez, BA, Kevin A. Wu, BS, Kevin M. Klifto, DO, PharmD, Tyler S. Pidgeon, MD, Christopher S. Klifto, MD, and David S. Ruch, MD
DOI: https://doi.org/10.1016/j.jhsa.2024.02.001
Summary
The authors sought to determine what evidence there is in well-designed studies in the literature, supporting the use of hyaluronic acid (HA), platelet rich plasma (PRP) and corticosteroid in the non-operative treatment of osteoarthritis of the trapeziometacarpal joint (TMJ OA). They assembled ten randomized controlled trials including 673 patients that compared pain score (visual analog scale) and a series of impairment measures including grip and pinch strength. In the sort and medium term, there were no differences in outcome between corticosteroid and HA. In the medium term, there was no difference in outcome between corticosteroid and PRP. Two studies that compared corticosteroid to saline injection did not report any differences in outcome. The authors conclude that in the absence of any clear advantages to HA and PRP, but costs and inconvenience related to the volume of injectate and the process of preparation of both HA and PRP, if an injection is considered in the non-operative care of TMY OA, it should use corticosteroid.
Points for discussion
- The study only included what were considered high level of evidence investigations, randomized controlled trials. What are some potential problems with that approach and are any of those mitigated by the strategy of meta-analysis?
- The manuscript addresses the fact that there was likely substantial variability in the nature of the corticosteroid used, but is that actually a reasonable concern if, overall, there were no advantages to the other injectates compared to a wide assortment of injected steroid compounds?
- What will it take for a lack of evidence supporting treatments that are expensive to supersede the requests of patients to receive them?
